



Professor Alister Hart and colleagues explore the 3D-CT planning software available to surgeons in the context of hip and knee arthroplasties
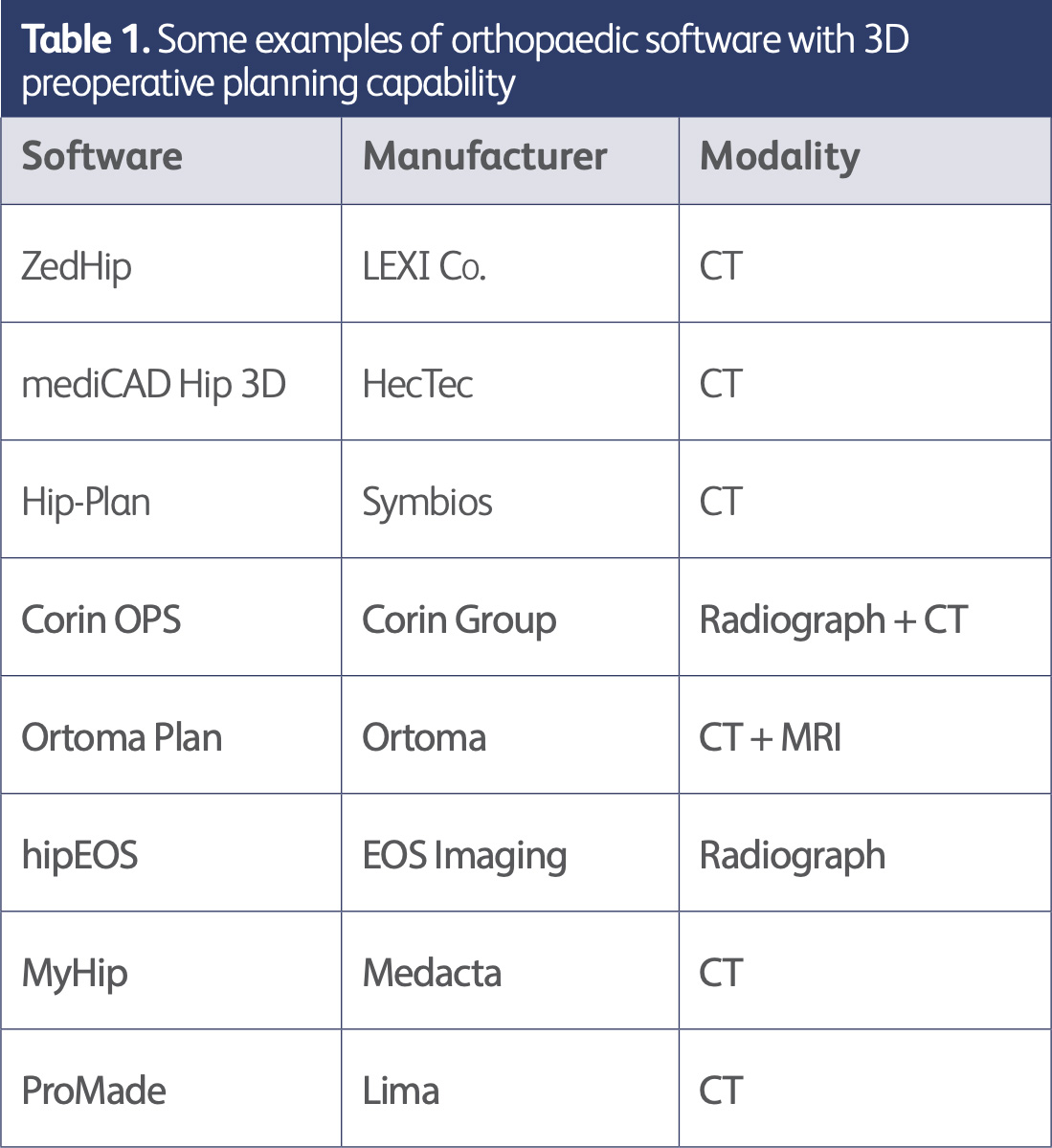
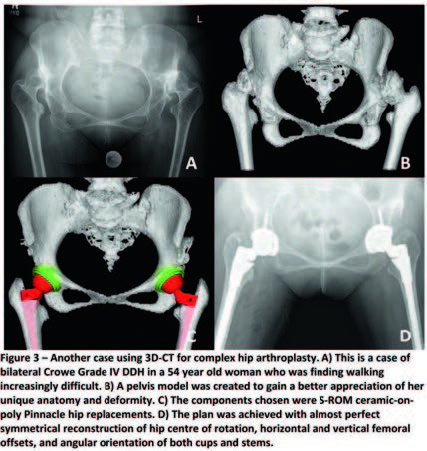
When was the last time you consulted a road atlas? Nowadays we use Global Positioning Systems (GPS) for navigation. Similarly, in orthopaedics, more and more surgeons are using specialised 3D-CT software to plan hip and knee arthroplasties, as the benefits of using such systems are becoming more recognised and CT technologies continue to improve. Some examples of commercially available CTbased 3D planning software include ZedHip (LEXI), mediCAD (HecTec), Hip-Plan (Symbios) and Ortoma Plan.
Although CT itself has been used for planning joint replacements for over 30 years [1], preoperative planning with 3D-CT is a more recent concept in orthopaedics. The surgical planning potential of 3D-CT was first explored for craniofacial surgery in the 1980s after it was found that 3D reconstructions could be generated from CT data [2,3].
Since then, two main surgical applications of 3D-CT in orthopaedics have been described. The first is 3D printing, where 3D-CT models can be used to create physical models that surgeons can hold in their hands and inspect [4,5]. These models may even be used to simulate surgery and for training purposes. The second is dedicated planning software that surgeons can feed patients’ CT data into and produce detailed 3D-based surgical plans; these computed plans can then be modified and adjusted by surgeons according to what they deem to be best for the individual patient [6,7]. This article will discuss planning software primarily in the context of hip and knee arthroplasties.
The conventional method of planning hip and knee arthroplasties is plain radiograph templating, which involves superimposing a template film over plain acetate radiographs to infer both the likely size and position of the implant [8,9,10]. With the advent of digital radiography and institution-integrated picture archiving and communications systems (PACS), there have been shifts towards digital templating as a more up-to-date alternative [11]. However, this technique may not be entirely accurate owing to the two-dimensional nature of templating and its uncertainties in representing three-dimensional bony structures [10, 11].
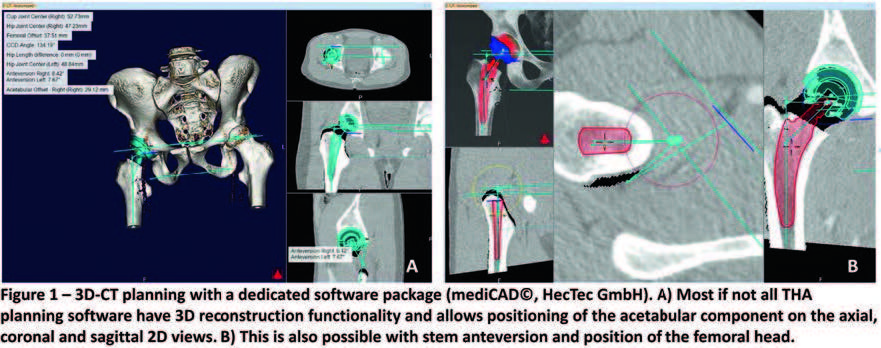
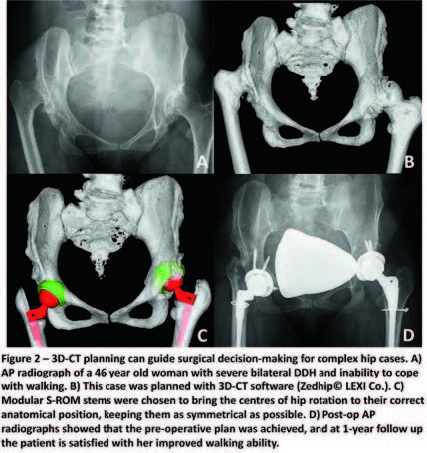
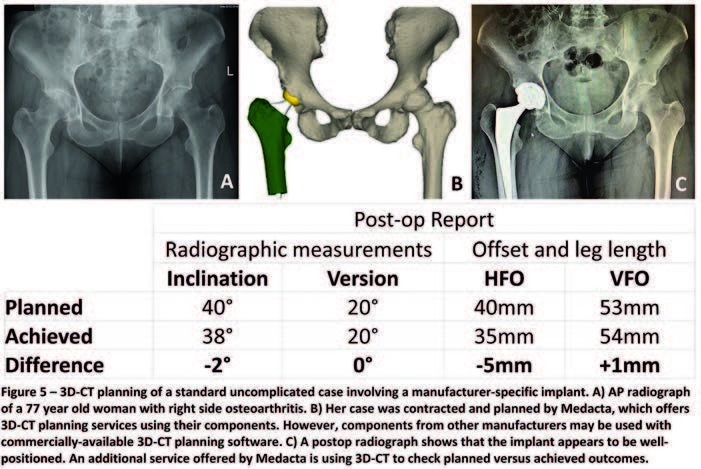
With 3D-CT software, a pelvic model is generated using the 2D slices of the patient’s CT scan. Subsequently, depending on the software, the likely component sizes may be computed by the programme, which the surgeon or radiologist can size up or down and reposition within the model to achieve a best fit. This has been shown to reduce intraoperative guesswork when it comes to choosing component sizes for both acetabular and femoral components in total hip arthroplasty [6,12-14]. This is particularly useful for less-experienced orthopaedic surgeons as 3D-CT plans help automate and increase accuracy during the process of implant selection [13, 15]. Most planning software also calculate values such as cup orientation and femoral neck anteversion, allowing surgeons to check whether these plans meet the correct parameters. Overall, there is evidence to suggest that 3D-CT planning enhances surgical precision of joint replacement surgery [16].
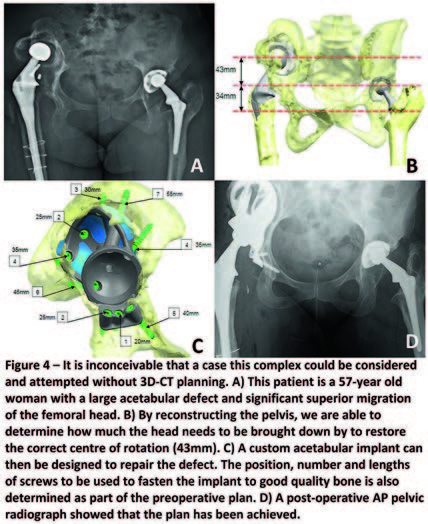
As a three-dimensional construct, 3D-CT plans are considered to be a better map of the patient’s anatomy and measurements taken are generally more accurate [17]. Being able to visualise pelvic anatomy ex-vivo allows surgeons to appreciate the patient’s unique anatomy in a way that would not be possible with standard medical imaging, giving them a more concrete idea of what to expect before the operation. This may help surgeons anticipate potential intraoperative complications, such as femoral fracture and leg length inequality [18].
mehr lesen
mehr lesen
mehr lesen
Another large barrier to widespread use of 3D-CT planning is the learning curve associated with new technology and systems. Specialised software often involves many complex steps to attain what appears to be a simple function – for instance, 3D pelvic modelling for many planning systems requires specific anatomical points to be selected, and the design of user interfaces can appear daunting to approach at first glance. As such, it may be difficult to convince radiologists and orthopaedic surgeons to invest effort and resources into familiarising themselves with the software, especially if the benefits are not readily apparent. Receiving training from manufacturers is one possible solution, but would be likely to come at an additional monetary cost.
This represents a sizable cost in terms of manufacturing large cases of instruments and implants, which are expensive to sterilise, transport and store.
With 3D-CT, as the implant sizes are better known to the surgeon, the volume of equipment normally made available for joint replacement surgery can be pared down to reflect the true sizes required by the surgeon to fit their patient. This allows for smaller, more compact sets of surgical tools that are easier to assemble and use. Further down the line, this can be made even more convenient for the industry and hospitals alike through developing disposable tools, which may be safer to use and more cost-effective in the long run.
mehr lesen
As software, the vast majority of 3D-CT planning systems are programmed to run on the Windows operating system. While this normally does not pose a problem due to the ubiquity of Windows, it is still worth considering potential difficulties faced by medical institutions or professionals who prefer other computer operating systems, in which case even less 3D-CT planning software would be available.
Furthermore, there may be compatibility issues with regard to an institution’s CT scanning protocols and those required by some planning software. Often, CT acquisition parameters such as the collimation and type of bone reconstruction kernel must follow specific presets in order to produce scans that can be used with the software. Hence, existing imaging and scanning protocols would need to be reviewed prior to distribution of 3D-CT planning systems throughout an institution.
As is generally the case with all medical imaging, there is the concern of increased radiation exposure for patients undergoing CT investigation for 3D planning. Best medical practice dictates that patient radiation exposure should be kept as low as reasonably possible [19], and hence there is a need for CT scanning protocols that both fulfil the requirements set out by planning software and restrict radiation dose to a minimum.
mehr lesen
In this section we will discuss the innovations that are vital to successful 3D-CT planning and their likely improvements in the near future.
The use of 3D-CT planning may now be considered a feasible option in contemporary orthopaedic practice where it may not have been possible a decade ago. This is largely due to better and more widely available CT scanners that can capture bony geometry at a higher spatial resolution and reduced noise, producing scans of sufficient quality to perform 3D reconstructions with. Modern scanners are also able to image patients much more quickly than before, reducing patient discomfort and radiation exposure [20]. Future improvements to CT scanners will no doubt further increase the viability of employing 3D-CT planning on a large scale than what currently exists.
mehr lesen
Recent advances in low-dose CT technology tailored for the specific purpose of planning orthopaedic surgery have made justifying the radiation burden to the patient and surgeon considerably easier. The new imaging protocols include imaging the hip, knee and ankle regions at a comparatively lower effective radiation dose without a significant tradeoff in image quality [21,22,23]. These protocols have seen a four-fold reduction in radiation equivalent to one year of background radiation, and have been enhanced further by the introduction of orthopaedic metal artefact reduction (MARS) sequences on many modern CT scanners, allowing suppression of noise produced by pre-existing metal implants [24,25]. This is especially important when planning revision surgery with 3D-CT, as the presence of excessive metal artefact will render 3D reconstruction impossible.
Radiographers in many orthopaedic units are now trained to operate CT scanners with both low-dose protocols and MARS sequences, which has partly set the groundwork for wider rollout of 3D-CT planning. The next possible steps include surgeon-specific CT protocols that radiographers can input into CT scanners and interchange with ease, and optimising 3D-CT planning software for compatibility with low-dose scanning parameters in mind.
mehr lesen
Radiologists often work closely with orthopaedic surgeons to provide necessary medical images for preoperative planning. An extended partnership would ideally see radiologists who are able to use 3D-CT planning software to help orthopaedic surgeons plan cases on request, especially busy surgeons who may not be familiar with the software. To streamline this process, radiologists should be trained in the use of planning software, and there should be an institute-approved standard operating procedure detailing the steps for handling cases, from receipt of CT data to delivery of the surgical plan.
Ergonomics should be a key consideration in the future design of planning software; the learning curve for new technology is often steep and it is more likely that medical professionals will embrace and become accustomed to using the planning software if it is as user-friendly as possible – this may be accomplished through minimalistic user interfaces with clear labels as well as integrated video tutorials on the software’s available functions. In an ideal scenario, all 3D-CT planning software would be intuitive enough that even surgeons with little to no technical experience with the software would still be able to generate a basic plan.
mehr lesen
3D-CT planning is the first rung on the ladder to better implant surgery, opening up a world of benefits to surgeons, patients, industry and hospitals. The benefits include quicker and more accurate surgery, better functional outcomes for patients and a push towards the development of an optimal inventory of implants and tools for joint replacement surgeries. It is a modern approach to the conventional planning process, which has been very much akin to navigating roads with a paper map. With the most sophisticated and current technologies available to us, 3D-CT is a promising field in which many more developments can be expected.
mehr lesen
mehr lesen
