



Lorem ipsum dolor sit amet, consetetur sadipscing elitr, sed diam nonumy eirmod tempor invidunt ut labore et dolore magna aliquyam erat, sed diam voluptua. At vero eos et accusam et justo duo dolores et
Veröffentlicht am, 30.08.2022
Preoperative planning of Total Hip Arthroplasty. Must this essential part of the
procedure be necessarily performed by the orthopedic surgeon?
A prospective study about 100 Corail® Hip System
Thierry Thirion, Pierre Georis, Zoé Szecel, Philippe Gillet
From the University Hospital Sart-Tilman, Orthopaedic Department, Liège, Belgium
Currently, patients who undergo total hip arthroplasty want a complete restoration of their hip function and not only pain relief. Templating in THA is essential for accurately predicting the optimal size of the implants required. It also reduces the risk of potential complications. To check the reproducibility of our preoperative planning, to compare the accuracy of templating
between orthopedic surgeon (OS), orthopedic resident (OR) and data manager (DM), to determine the learning curve between the different planners and to evaluate the effect of body mass index impact on digital templating for THA. One hundred uncemented Corail® Hip System using a ceramic on ceramic bearing surface were included into the study. The software used for templating was
IMPAX-Orthopaedic-Tools. A calibration marker (28-mm ball) was used for calibration. All the anteroposterior pelvis radiographs were planned by three participants (OS, OR, DM).
We systematically collected the precisely planned size measurements as well as the variation by 1 or 2 sizes of prostheses. At +/- 1 size, we did not find any significant difference between the participants with respectively 94%, 96% and 93% concordance for the cup, 88%, 90% and 90% for the stem and 85%, 84% and 83% for the neck.
Our preoperative templating was accurate in predicting the required implant size and results were similar to those available in the literature. We did not find any difference between the planners and we were unable to objectivate a learning curve period.
No benefits or funds were received in support of this study. The authors report no conflict of interests.
We conclude that this essential part of the planning procedure can be performed by the surgeon himself or an orthopedic resident or a data manager who has anatomical knowledge if the surgeon is unable to perform templating himself.
Keywords : THA digital templating ; THA preoperative
planning ; 2D planning
Total hip arthroplasty (THA) is a common and successful treatment for patients suffering from severe osteoarthritis. THA has been considered as “the operation of the last century” (1).
The rate of total hip arthroplasty increased over the last years. Younger and more active patients are operated. Optimal surgery outcome is the desired goal (2).
Correspondence: Dr Thierry THIRION, University Hospital Sart-Tilman, Orthopaedic Department, B-4000 Liège, Belgium.
Fax : +3243667537.
E-mail : tthirion@chuliege.be © 2020, Acta Orthopædica Belgica.
The targets of surgery have evolved from pain relief to full restoration of function through correction of any limb length or offset discrepancy and optimal soft tissue tensioning. Digital
preoperative templating has been described to be an accurate and reproductible process for the planning of THA (3).
By the implantation of prosthetic components, the reconstruction of the hip will also affect the constraints, the joint stability and long-term survival rate of the implants. The literature reports that a decrease or increase of more than 5 mm in offset can negatively affect the wear of the contact surfaces by increasing the joint reaction forces (4).
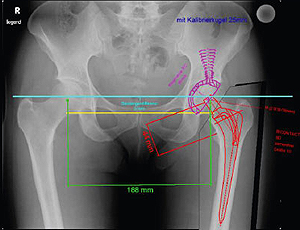
In addition to patient’s clinical examination, preoperative planning requires a digital pelvis x-ray in which a calibration tool is mandatory for accuracy. Templating in THA is an essential part of the procedure to reduce the risk of potential complications. Benefits include estimation of appropriate acetabular and femoral component size for uncemented protheses to avoid subsidence with too small components or fracture with oversized components. Templating decreases surgical time (5).
The success of preoperative planning can be measured using both objective and subjective outcome measures (2). Before the introduction of digital radiographs, templating typically involved the use of analog radiographs and acetate inlay templates (6). Classically, templating is performed using a plain anteroposterior x-ray of the pelvis centered on the symphysis pubis (7).
Templating techniques have been considerably improved with the introduction of digital radiographs. The application of radio-opaque markers to calibrate the digital radiograph is the standard
method in templating softwares (8). Ramme et al (5) have demonstrated the importance of proper position of scaling markers for accurate digital templating for hip surgery. Placing the
scaling marker 3.5 cm more anterior or posterior of the center of an acetabular implant resulted in one cup size difference from the actual implant size (5). To accurately scale the image, the scaling marker must be placed as close as possible to the anatomical region being x-rayed. Placement of a scaling marker is difficult when the region of interest is deep within
soft tissue. The most accurate digital templating is achieved when scaling markers are positioned as close as possible to the center of the hip joint (5). The aim of the present study is to compare the accuracy of preoperative templating between an orthopedic surgeon (OS), an orthopedic resident (OR) and a data manager (DM). We analyse the reproducibility of the templating in order to determine the learning curve between the different planners, and we search the effect of body mass index (BMI) impact on digital templating for THA.
MATERIALS AND METHODS Between January 2016 and March 2018, one hundred uncemented Corail® Hip System (DePuy Orthopaedics INC, Warsaw, IN, USA) protheses were implanted into 93 patients. Sex ratio male/ female was 39 :54 with a mean age of 66 (range 31 to 90) years at the operation. All the patients were included into the study. The mean BMI was 24.35 (range 16.16 to 41.65). The ASA score was I in 10, II in 88 and III in 2 patients. The surgical indication was osteoarthritis in 88%, avascular necrosis in 9% and femoral neck fracture in 3% of the cases.
All the THA were performed using a posterolateral approach with the patient positioned in lateral decubitus using standard positioners without fluoroscopy. All THA were performed by the same
surgeon in the same hospital. The software used for templating was IMPAXOrthopaedic-Tools Version 3.0.2.3 (Agfa Healthcare N.V. Mortsel, Belgium).
A calibration marker (28-mm ball) was positioned between the thighs of the patient at the anteroposterior level of the greater trochanter. All the anteroposterior pelvis radiographs were
planned by three independent operators (OS, OR, DM). The implanted stem was a Corail® collared standard offset 135° neck angle (KA) in 18, a Corail® collared Coxa Vara 125° neck angle (KLA)
in 77 and a Corail® collarless high offset 135° neck angle (KHO) in 5 patients (Table I).
Table I. — Number of stems implanted by size
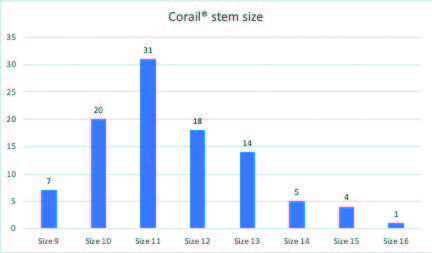
Table II. — Number of cups implanted by diameter
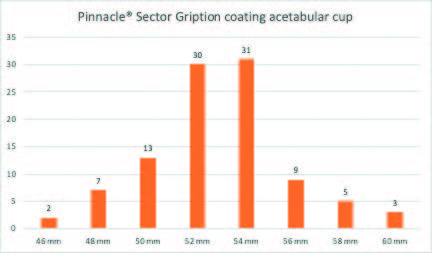
Table III. — Number of prosthetic heads implanted by diameter
All patients received a press-fit Pinnacle® Sector Gription coating acetabular cup (DePuy Orthopaedics INC, Warsaw, IN, USA) (Table II).
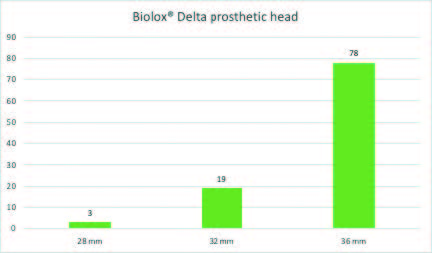
The insert used in all cups was a Ceramax® Biolox® Delta (DePuy Orthopaedics INC, Warsaw, IN, USA) combined with a Biolox® Delta (DePuy Orthopaedics INC, Warsaw, IN, USA) prosthetic head (Table III).
RESULTS
All results are expressed in size agreement between the planned implant and the prosthetic component actually implanted as well as for cup, stem and neck length of the ceramic prosthetic head.
We systematically collected the precisely planned
Table IV. — Cup size agreement (planning/implantation) in percent calculated by different observers
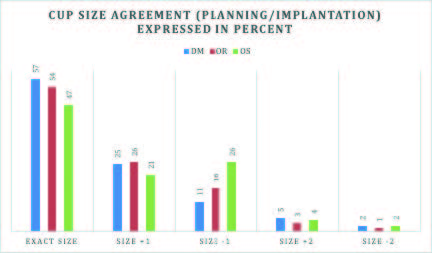
Table V. — Type of stem agreement (planning/implantation) calculated by different observers
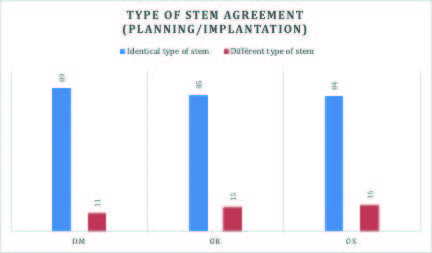
Table VI. — Stem size agreement (planning/implantation) in percent calculated by different observers
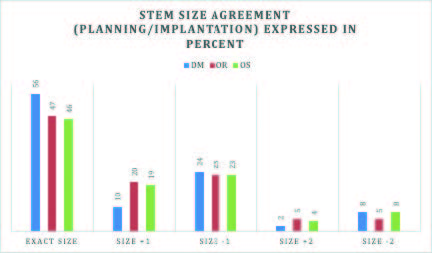
Table VII. — Neck length agreement (planning/implantation) in percent calculated by different observers
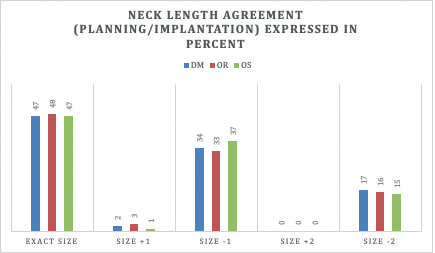
Table VIII. — Interobserver comparison for the cup (planned/implanted)
| DM | OR | OS | |||
|---|---|---|---|---|---|
| Exact Size | 57% | SD | 54% | SD | 47% |
| +/- 1 Size | 93% | NSD | 96% | NSD | 94% |
| +/- 2 Sizes | 100% | NSD | 99% | NSD | 100% |
| At +/- Size | DM/OR | P=0,261 | |||
| DM/OS | P=0,347 | ||||
| OR/OS | P=0,343 |
Table IX. — Interobserver comparison for the stem (planned/implanted)
| DM | OR | OS | |||
|---|---|---|---|---|---|
| Exact Size | 56% | SD | 47% | SD | 46% |
| +/- 1 Size | 90% | NSD | 90% | NSD | 80% |
| +/- 2 Sizes | 100% | NSD | 99% | NSD | 100% |
| At +/- Size | DM/OR | P=0,439 | |||
| DM/OS | P=0,526 | ||||
| OR/OS | P=0,343 |
Table X: Interobserver comparison for the neck (planned/implanted)
| DM | OR | OS | |||
|---|---|---|---|---|---|
| Exact Size | 47% | NSD | 48% | NSD | 47% |
| +/- 1 Size | 83% | NSD | 84% | NSD | 85% |
| +/- 2 Sizes | 99% | NSD | 99% | NSD | 99% |
Table XI: Implants size agreement (planned/implanted) between observers (in percent)
| Cup | Stem | Neck | |
|---|---|---|---|
| Exact Size | 44% | 45% | 87% |
| +/- 1 Size | 93% | 96% | 100% |
| +/- 2 Sizes | 100% | 100% |
size measurements as well as the differences up to 1 and 2 sizes (Tables IV, V, VI and VII). Regarding the interobserver comparison, we did not show any significant difference (SD) in terms of
planned cups and stems compared to the prostheses truly implanted up to a variation of +/- 1 size (Tables VIII, IX, X, XI). The detailed analysis of our planning results did
not show any learning curve for the cup, the stem and the neck of the prosthetic head.
Discussion
Digital templating of THA is an important step of the procedure. Two-dimensional method is accurate but the planning softwares are expensive and then only used on in hospital computers. Sometimes, it is impossible for the orthopedic surgeon to perform this procedure on time. The main purpose of the present study was to compare the accuracy of preoperative
templating between different operators, to check the reproducibility of our templating, to determine a potential learning curve and to research the effect of BMI on digital templating for THA. There was no correlation with severity of arthritis on radiograph and accuracy of templating in our series. During the procedure, the surgeon chooses the cup that requires a minimal amount of reaming of the native the acetabulum and the stem that restores the optimal natural offset of the hip. Numerous studies determine the precision of digital templating by comparing the templated and the truly implanted stems and cups (9-14). However, this approach ignores the effect of the experience of various operators on templating as well as individual intra-operative decisions made in regards to component size. These studies did not compare the templating results between different operators like orthopedic surgeon, orthopedic resident and data manager that has some experience in THA planification and follow-up. Regarding to our results, we did not find any difference whatever the planners. Our preoperative planning was similar with those available in the
literature. We did not highlight a learning curve period.
Jung et al (15) showed that a lower level of experience in templating has no effect on the planning results of the acetabular components, but there were considerable and significant differences when planning the femoral components. The design of the stem had an impact on planning accuracy in their study (15).
Hsu et al (16) studied the effect of training level on the accuracy of digital templating for primary THA. Interobserver reliability for templating THAs
showed good results. The intraobserver reliability was excellent or good (16). Strøm et al (17) found that the precision of an uncemented THA templating does not rely on the professional experience. They found no association between increasing experience and improved precision, as the least experienced observer showed the highest intraobserver reliability (1).
Templating of THA is an essential step in elective joint replacement surgery ; its importance is generally accepted. The introduction of digital radiographs and templating has led to the necessary use of spherical external calibration markers. A precision of ± 1 component size between preoperative templating and implanted component has been defined acceptable (8).
Kumar et al (18) found that templating the acetabular cup had 56% accuracy, 91% to with 1 size, and 100% to within 2 cup sizes. There was 62% femoral stem accuracy and 78% to within 1
size. The femoral offset was accurately predicted in 93% of the cases (18).
In 2010 Gamble et al (19) showed that digital templating uncemented THA and accurately predicted the cup size in 38% of the cases and 80% to within 1 cup difference. The accuracy of the femoral stem was 35% and 85% to within 1 size (19). In the study of Riddick et al (11), the cup and stem sizes were predicted correctly (within one size error) in 87% and 92% of the patients respectively (11). Shaarani et al (3) have demonstrated exact accuracies to be 38% in the acetabular component and 36% in the femoral stem. The accuracy to within 1 size in the acetabular or femoral components, which was comparable with other studies (3). Using digital templating, Shemesh et al (12) predicted the exact acetabular cup size in 41% of posterior approach (PA) cases. For PA hips, a total of 88% of cup sizes were predicted within +/- 2 mm (1 size), and 99% were predicted to within +/- 4 mm (2 sizes) (12). Sershon et al (20) showed that for the acetabular
component, digital templating was accurate in predicting the final implant size in 64.5% of THAs (20). Digital templating was within 1 size for 93.0% of THAs. In their study, there was no correlation between BMI and the planned cup size. For the femoral component, digital templating was accurate in predicting the final implant size in 45.7% of THAs. Digital templating was within 1 size for 82.0% of THAs. There was no correlation between BMI and stem size planned (20). Our study showed that we did not showed any significant difference between the participants with respectively 94%, 96% and 93% concordance for the cup, 88%, 90% and 90% for the stem and 85%, 84% and 83% for the neck at +/- 1 size. Our results are in concordance with those presented in the listed literature (3, 10-12, 18-20). As Kniesel et al (10), we were unable to find any evidence of interdependence between planning accuracy and BMI in the planning of THA.
CONCLUSION
Digital templating is an efficient method to predict the final component sizes in THA. Our preoperative digital templating using a calibration marker positioned between the thighs of the patient was accurate in predicting the implant size. We did not find any difference whatever the planners and we were unable to identify a learning curve period.
In this study, the effect of body mass index has no impact on the accuracy of digital templating for THA.
Although the planning of a total hip arthroplasty should preferably be performed by the surgeon, we concluded that this essential part of the planning procedure can also be performed by an orthopedic resident or a data manager who has anatomical knowledge.
REFERENCES